Jordi Sanchez-Ballester
FRCSEd FRCS Trauma & Orth
Consultant Foot, Ankle & Knee Surgeon
Fairfield Independent Hospital, St Helens
Spire Cheshire, Whiston & St Helens Hospitals
Bone-Surgeon.co.uk
Fairfield Independent Hospital
Crank Rd
St Helens
Merseyside WA11 7RS
01744 739311
Spire Cheshire Hospital
Chris Davies
Fir Tree Close
Warrington WA4 4LU
0845 602 2500
How Do Knees Work?
Sitting, standing, running, walking, squatting to pull a weed in your garden or jumping to shoot a basketball are all made possible by the knee's ability to bend and flex. The knee is one of the most complex joints in your body, and it uses a combination of bones, muscles, ligaments and tendons to work.
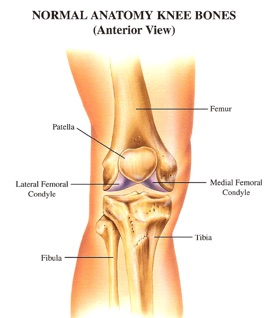
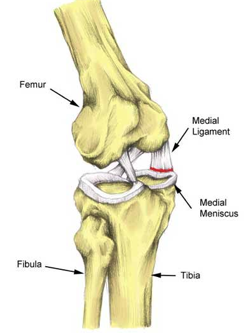
Parts of the Knee
Your knee is made of the femur (thighbone), the tibia (shinbone) and the patella (knee cap), which sits over the knee to protect the joint. The fibula, the bone that runs parallel to the tibia in your lower legs, connects to the tibia immediately below the knee but is not part of the joint. Ligaments, bands of elastic tissue, attach these bones together.
The anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL) are the two main ligaments in your knee. (These are sometimes referred to as crucial ligaments.) These ligaments attach the tibia to the femur and help control the forward and backward motion of the knee and also keep it from rotating too far.
Strong cords of tissue, called tendons, attach muscles to the bones of the knee and make it possible for the joint to move. The main muscles involved in knee movement are the quadriceps and the hamstrings.
Your quadriceps are a group of four muscles on the front of your thigh that are attached to the top of the patella by the quadriceps tendon. The hamstring muscles, located on the back of your thigh, are connected by ligaments to the tibia just below the knee joint.
Common Knee Problems - Patella and Quadriceps Tendinitis
Patella tendinitis is a common injury following overuse or repetitive trauma to the extensor mechanism, such as basketball or volleyball. Patients usually present with pain in the front of their knee over the patella tendon associated with limited flexion and swelling.
Treatment is directed towards a period of rest to allow the symptoms to subside followed by activity modification that limits high impact sports.
Stretching and strengthening exercises are initiated once the pain subsides. Ice and short courses of NSAID's are helpful adjuncts.
In a similar fashion, the quadriceps tendon may become sore and irritated. This is usually manifested with tenderness in the soft tissue just above the patella. Treatment is similar to patellar tendinitis as discussed above.
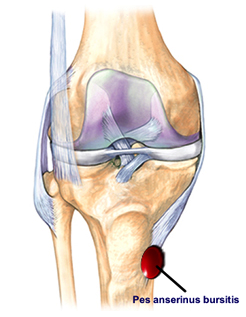
Bursitis
Bursae are synovial lined cavities that overly a bony prominence around the knee. Repetitive trauma from overuse or, more commonly, chronic irritation results in local inflammation and fluid collection within the bursa. The prepatellar bursa is the most commonly affected and when inflamed is called "housemaid's knee."
The bursa overlying the attachment of the medial hamstrings or pes anserinus tendons on the tibia can also become inflamed. This is usually termed a pes bursitis and is usually caused by a repetitive activity such as running.
Treatment is directed at stopping the irritating activity.
Ice and a short course of NSAID's are useful. A compressive wrap is sometimes helpful. Aspiration is sometimes required for extreme cases.
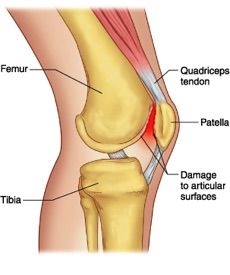
Patellofemoral Pain and Chondromalacia Patella
Pain in the front of the knee is a common complaint and can be the result of numerous maladies. Sources of pain include patella malalignment, chondromalacia, osteoarthritis, osteochondral fractures, synovial plica, bursitis, tendinitis, and patella instability.
An understanding of knee anatomy, as it relates to the mechanism of injury, is important in establishing a diagnosis. Your physician may need to perform ancillary tests in order to finalize a diagnosis. While the initial treatment is usually nonoperative, it is sometimes necessary to perform surgery to solve the problem.
Malalignment, along with acute or repetitive trauma, can lead to degenerative changes on the surface of the patella or femoral groove. Softening and erosive changes are referred to as chondromalacia. Initial treatment includes activity modification, ice and NSAID's.
As the pain subsides, an exercise program is begun that usually focuses on stretching and strengthening. For those patients with recalcitrant cases, their physician may need to modify their treatment plan and consider surgical intervention.
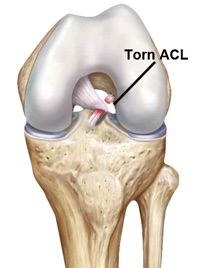
Anterior Cruciate Ligament Injuries
ACL tears are becoming more common, with an incidence of 250,000 cases per year in the United States. Women experience up to a sevenfold increase in ACL tears compared with men in competitive sports. The ACL is often torn during running sports when the foot is planted and the knee twists with a change of direction.
Classically the individual feels a "pop" in the knee, and is unable to continue running or playing because of pain and a sense of instability. Besides a physical examination and x-rays, it may be necessary to perform a MRI to confirm the diagnosis.
Treatment may be either operative or nonoperative and is dependent upon the individual's level of activity and degree of instability. It is important that the individual be counseled about the natural history of an ACL deficient knee by their patient before embarking on a course of treatment.
Nonoperative treatment involves a physical therapy program for restoration of motion and strength. Most athletes return to sports in 6- 8 weeks provided that they have achieved appropriate strength.
The use of a brace is debatable, but may provide some subjective benefit. If an athlete suffers episodes of giving way with sports, then it should be assumed that the knee is functionally unstable and reconstructive surgery should be considered.
Current reconstructive techniques use an arthroscopic approach. The graft choices for an ACL reconstruction include the central one-third bone-patella tendon-bone; hamstring tendons and quadriceps tendon. Sometimes, allograft tissue is considered.
Following the reconstructive procedure, a supervised and specialized rehabilitation program is necessary to restore motion and strength.
In general most athletes return to sports by 6 to 9 months after surgery, but each case is individualized.
Posterior Cruciate Ligament Injuries
PCL injuries occur less often than ACL tears. Two common mechanisms of injury include a fall on a hyperflexed knee with the foot plantar flexed and striking the front of the tibia with the knee flexed - like a dashboard injury in a motor vehicle accident.
Treatment may be operative or nonoperative depending upon the degree of instability and involvement of associated structures.
Meniscal Tears
Meniscal tears usually result from a twisting injury. Because the medial meniscus is less mobile than the lateral meniscus, it has a greater chance of being entrapped between the femur and tibia in the knee joint.
Beyond the physical exam and x-rays, MRI has been useful in confirming the diagnosis.
While some meniscal tears may heal with rest and activity modification, failure to respond to nonoperative treatment or repetitive episodes of catching or locking suggest that a surgical arthroscopy should be considered.
Depending on the pattern and extent of the tear, the arthroscopy may involve either a partial menisectomy or meniscal repair.
Following arthroscopy, an exercise program facilitates restoration of motion and strength.